Do insurers take into consideration the severity of peripheral vascular disease when evaluating applicants?
Other related medical conditions (or medical terminology) include Peripheral Vascular Disease, Peripheral Artery Disease, Carotid Artery Disease, Arteriosclerosis, Blocked Arteries. Read below for more information about Peripheral Vascular Disease and receiving a life insurance quote from a life insurance specialist.
What Is Peripheral Vascular Disease?
The body’s circulatory system consists of two types of blood vessels, the arteries and veins, which carry blood throughout the body in the following cycle: Arteries carry blood rich in oxygen and nutrients from the heart to the organs and cells; the veins carry oxygen-depleted blood and waste through the kidneys, liver, and lungs, where waste is filtered out and removed from the body. The venous blood is then again filled with oxygen in the lungs and returns back to the heart. This pipeline of arteries and vessels is interconnected by smaller blood vessels called capillaries.
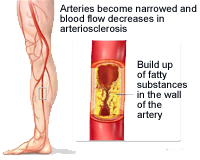
Peripheral artery disease, which causes plaque forming arteriosclerosis that blocks, narrows, or weakens the vessel walls, is the major underlying cause for peripheral vascular disease. When arteriosclerosis hardens the arteries of the heart it is referred to as coronary artery disease, but when it affects the arteries that supply the legs and feet, the renal arteries leading to the kidneys, and the carotid arteries in the neck that lead to the brain and arms it is referred to as peripheral vascular disease. In addition to arteriosclerosis, blood vessel narrowing can occur due to blood clots (thrombus/emboli) that block blood vessels; complications from diabetes; inflammation due to arteritis or vasculitis; infection from Salmonella bacteria or syphilis; structural birth defects or injury.
More than Aching, Tired Legs
Symptoms of peripheral vascular disease in the lower region of the body commonly appear first in the legs and feet. Pain, called ischemia, occurs when muscles receive an insufficient supply of oxygen rich blood due to an artery’s inability to dilate and accommodate greater blood flow when needed or when it is totally blocked. Upon physical examination, the presence of the following symptoms may point to peripheral vascular disease:
- Burning or aching pain in the fee or toes while at rest
- Buttock pain
- Change of color of the legs
- Cold legs or feet
- Dry, fragile or shiny looking skin
- Impotence
- Leg pain (occurs with exercise/relieved with rest) called intermittent claudication
- Loss of hair on the legs and/or feet
- Muscle pain in the thighs, calves, or feet
- Numbness of the legs or feet at rest
- Paleness or blueness (cyanosis) of skin
- Pulse is weak or absent in the limb
- Sores that do not heal
- Walking/gait abnormalities
Peripheral vascular disease in the carotid arteries may cause temporary weakness or numbness of the face, arm and/or leg on one side of the body, temporary loss of speech, trouble speaking or understanding speech, temporary loss of vision or dizziness and unsteadiness or sudden falls. If renal peripheral vascular disease is suspected, blood pressure may be elevated and kidney dysfunction will be evident.
Peripheral Vascular Disease- Diagnosis and Treatment
When peripheral vascular disease is suspected, there are several tests that will verify the diagnosis:
- Ankle/Brachial Index (ABI) compares the blood pressure in the arm (brachial) with the blood pressure in the legs. An ABI above 0.90 is normal; 0.70-0.90 indicates mild peripheral vascular disease; 0.50-0.70 indicates moderate disease; and less than 0.50 indicates severe peripheral vascular disease.
- Treadmill Test: Blood pressure in arms and legs is taken before and after exercise. A significant drop in leg blood pressures and ABIs after exercise suggests peripheral vascular disease. If the leg pulses are not palpable, the use of a portable Doppler flow probe will quickly reveal the absence or presence of an arterial flow.
- Angiography, or arteriography, is a type of x-ray that utilizes injected dye in the arteries to highlight blockages or narrowing of arteries on an x-ray. It is an invasive study performed in a catheterization or interventional radiology laboratory and is considered the best test available for this condition
- Ultrasonography is a less invasive form of imaging that uses sound waves to locate abnormalities. A handheld device that emits ultrasound waves is placed on the skin over the part of the body being tested. The waves “bounce” off structures under your skin and give an accurate picture of any abnormalities in the vessels. Obstruction of blood flow can also be seen.
- Magnetic Resonance Imaging (MRI) is a non-invasive x-ray that uses a magnetic field to obtain an image of internal structures. It gives a very accurate and detailed image of blood vessels.
Once a diagnosis is made, there are many treatment options to improve blood flow to organs and muscles affected by peripheral vascular disease. The severity of the condition will dictate the treatment plan.The least invasive treatment is with medication to control the disease and prevent worsening of the condition or complications in patients with hypertension or diabetes, those with high fat or lipid counts and those who smoke.
Medications may include pain relievers, blood thinners or drug therapy to dilate the affected artery or arteries and manage pain.
When circulatory improvement or pain management cannot be achieved with medicine, there is an invasive, but non-surgical procedure that can be performed during a diagnostic angiogram. When blockages are identified, specialists called interventional radiologists or invasive cardiologists can perform a procedure called balloon angioplasty to widen the artery. A thin plastic tube called a catheter is inserted into the affected artery through a needle under local anesthesia and X-ray dye or contrast is injected, x-ray films are taken and studied by the doctor. If the obstruction is significant, especially in a larger more proximal artery, angioplasty may be reasonable.The angioplasty catheter has a tiny balloon attached to the end. When the balloon is inflated, it pushes aside the plaque and widens the artery so that it no longer restricts blood flow. The balloon is then deflated and removed from the artery. Sometimes a stent, an open tubular structure made of plastic or steel, is inserted into an artery to keep it from becoming blocked again.
Surgery is usually reserved for severe cases when the disease is impeding a person’s ability to work or pursue activities of daily living. Surgery options may include endarterectomy to remove the lining of the artery, grafting to repair or replace the vessel or, most commonly, bypass surgery using a vein or synthetic graft. In severe cases, some people with peripheral artery disease may require surgical amputation of an affected limb.
Adopting a lifestyle that promotes heart health will help prevent peripheral vascular disease from progressing and may even reverse some symptoms. Eating a diet that is low in fat and cholesterol will improve vascular health and assist in maintaining a healthy weight.Managing high blood pressure and high cholesterol is imperative as arteriosclerosis is at the root of this illness. An exercise plan of walking or other activity, performed to the point of pain and alternated with rest periods, is often recommended. Over time this pattern of exercise will improve circulation because of the development of collateral (new, small) blood vessels that occur as a result. Smoking constricts arteries, decreases the blood’s ability to carry oxygen and increases the risk of forming clots so smoking cessation is mandated. Diabetics with peripheral vascular disease have special foot care needs. Shoes must fit properly. Careful attention should be paid to any cuts, scrapes or injury. The basic task of trimming your toenails warrants considerable care since injuring skin could lead to skin breakdown, gangrene, and loss of toes, if blood flow is impaired.
Better Disease Management Equals Better Insurance Opportunities
Applicants will need to share the date of diagnosis, the effect the disease has had on the heart, if any, and lifestyle, the treatment plan and how successfully symptoms are being managed. In addition, insurers will want a list of medications and dosages being taken to control symptoms and lifestyle changes being implemented to prevent disease progression. Smokers who quit will reap better insurance rates than those who do not. Persons who have coronary artery disease or any other type of heart disease, or severe claudication should anticipate higher rates.
How Can MEG Financial Help?
At MEG Financial, we have worked with many individuals across the country that have had related histories and have helped many obtain fairly priced life insurance. A number of these clients previously attempted to buy life insurance elsewhere but were either turned down or asked to pay a significantly higher rate. Our experience helping others with related problems is invaluable to you in identifying the insurance company that will treat you most fairly.
For more specific information or to obtain a custom quote, call MEG Financial today at (877) 583-3955. You may also submit this short form and an independent insurance agent will personally contact you to go over any questions or other concerns.

 Speak with an experienced advisor!
Speak with an experienced advisor! 


