Chronic Obstructive Pulmonary Disease and Life Insurance Rates
How COPD Affects Insurability
- Learning About COPD
- COPD Classifications and Treatment Options
- Getting Insurance When You Have COPD
- How MEG Financial Can Help
- Related Links for COPD
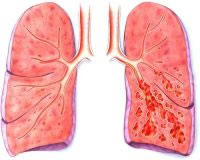
Learning about COPD
Individuals with COPD are living with a chronic disease process. Airway inflammation caused by chronic bronchitis can be managed with medications, but the damage to lung tissue from emphysema is permanent. Smokers who quit the habit once diagnosed can slow the progression of this disease.
There are several methods to diagnose COPD. Patients can be evaluated using chest x-rays and scans or with blood work, however the best indicator is accomplished with a series of Pulmonary Function Tests (PFT). The PFT evaluates how much air your lungs can hold, how quickly you can move air in and out of your lungs, and how well your lungs add oxygen and remove carbon dioxide from the blood. These tests can be used to help determine the cause of a person’s breathing problems and identifies those at high risk for developing lung disease. They also measure the lung function of a person who has lung disease and monitor the effectiveness of treatment. These tests are administered before surgery to determine a person’s ability to breathe or can be used to monitor the lung function of a person who is regularly exposed to substances that can damage the lungs. PFT measures the following lung values:
- Tidal volume (VT) which measures the amount of air inhaled during a normal breath.
- Vital capacity (VC) which measures the maximum amount of air you can exhale after you inhale as deeply as possible.
- Forced expiratory volume (FEV) which measures the amount of air you can exhale forcefully in a sustained breath over a period of one second (FEV1); two seconds (FEV2) or three seconds (FEV3). The total amount of air you exhale during this test is called the forced vital capacity (FVC).
Classification of COPD and Its Treatment
Mild: Individuals with a mild chronic cough or who experience shortness of breath following moderate exercise are experiencing mild COPD. PFT studies may be near normal levels and x-ray abnormalities are generally not noted, however, the person may have an increased tendency to get respiratory infections. There is no standard treatment at this stage.
Moderate: Individuals who demonstrate increased coughing and shortness of breath during mild exertion are classified with moderate COPD. PFTs note decreased levels of lung functioning and x-ray studies of the chest frequently show abnormalities. Chest abnormalities are frequently present. Inhalers, used on occasion, help with symptom management.
Severe: Individuals who experience shortness of breath during daily activities of living and or during minimal exertion are dealing with severe COPD. A marked decrease in pulmonary function is evident on their PFTs. Chest x-ray and chest abnormalities are typically present. Treatment includes inhalers, steroids and other medications to manage symptoms.
Extreme: Individuals with extreme COPD are typically disabled and incapable of completing activities of daily living. Due to shortness of breath that occurs while at rest or during minimal exertion, these individuals are often homebound and requires oxygen support. PFTs reveal severely reduced pulmonary function and x-ray and chest abnormalities are very evident. Treatment includes rest at home, various medications and oxygen.
In addition to the treatments described, some patients benefit from lung surgery to remove parts of the diseased lung. Lung rehabilitation is often suggested to teach patients how to breathe in a different way to help them stay active. In sever cases of COPD, a lung transplant may be performed.
Getting Insurance When You Have COPD
When insurers evaluate a person with COPD there are several factors they consider. First, they need to know that the COPD patient is in overall good health aside from the COPD. They also need to know that a smoker has quit smoking since the time of diagnosis. They will request PFT scores from your physician. Patients classified as having extreme COPD will have the most difficult time being approved for insurance since they are most at risk for medical complications at a later time.

 Speak with an experienced advisor!
Speak with an experienced advisor! 


